At the end of 2019, the New Humanitarian listed the top 10 crises to watch into 2020. Number three and four on that list were “Infectious disease: antibiotic resistance and a stubborn anti-vaccine movement” and “Macro-economic turbulence: more risk for the most vulnerable”.
Just two months into 2020, the world is reeling from the COVID-19 pandemic. As the virus continues to spread, health systems around the world are overwhelmed, Australia faces almost certain economic recession, and unprecedented international and domestic movement restrictions are imposed.
In the West, many are faced for the first time with such austere times. But for people living in protracted wars, poverty, disease, disasters, displacement, social and political exclusion are the daily experience. Ben Elton from the New Humanitarian highlighted perfectly, “We are all fragile, but we are not equally fragile.”
As Hugo Slim put it, “The whole world is facing a humanitarian emergency, the COVID-19 pandemic. And this crisis will shape a new culture of emergency ethics.” Humanitarian emergencies require difficult ethical decisions to be made, such as who receives aid in resource constrained environments. For those of us in the Western world, restrictions to our freedom of movement is a new experience. But this disruption to our daily life must be prioritised accordingly in order to continue protecting those more vulnerable in our communities and globally.
What does this all mean for the humanitarian world and humanitarian leadership to support the 168 million people in need of humanitarian aid and protection in countries of political instability, refugee camps, and weak health systems?
Since the World Humanitarian Summit in 2016, the localisation of humanitarian aid has been a priority through the Grand Bargain. The 2019 review of progress toward the Grand Bargain commitments improvements in cash programming, reporting, needs assessments, financing and use of technology, facilitating some progress toward achieving the Grand Bargain commitments.
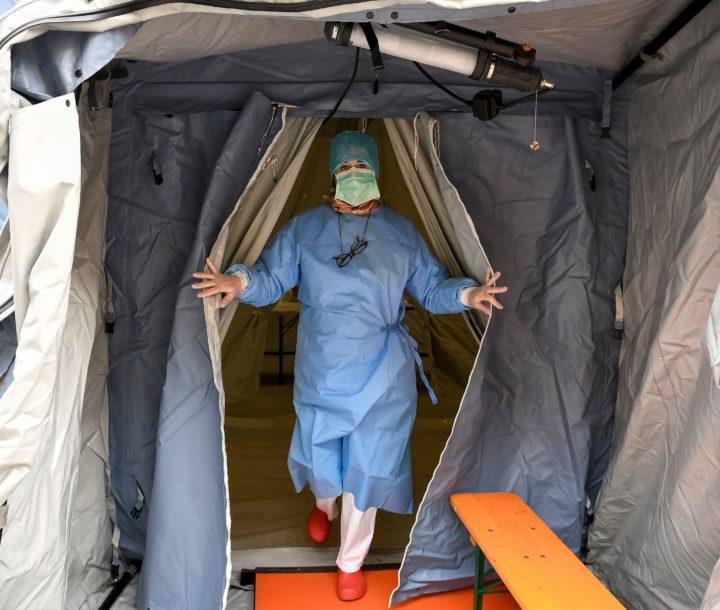
The question is how to protect staff and communities impacted by chronic crises in a world where remote management will become the norm. The increase of remote management is already happening, particularly in areas of long-term conflict and high insecurity, such as the Syria crisis. As remote management becomes more prevalent due to the COVID-19 pandemic, the leadership and support required from international humanitarian actors in program support, financial support, training and capacity building, and advocacy for equitable access to supplies such as personal protective equipment, tests and treatments must adapt.
Without question, the urgent need for public health systems strengthening is clear. No single public or private health system will be able to meet the demands that COVID-19 will bring.
Humanitarian actors have an opportunity to lead and advocate for the systems approach of rapid upskilling of healthcare workers and avoid developing parallel health systems and advocate and support the equitable distribution of medical supplies such as personal protection equipment. When effective vaccinations are available, how do we ensure that this is available to all people and not just the wealthy few.
Promoting and developing basic health literacy among health workers and affected communities will be critical. Providing accurate health information, and correcting misinformation, will be essential for humanitarian agencies. Challenging the stigma of humanitarian workers being vectors of the coronavirus, providing basic infection control messages, promoting the avoidance of mass gatherings, supporting testing, detection and surveillance efforts, while also contributing to the continuity of routine health services are essential to ensure that those with existing health issue such as diabetes and HIV have a continuity of care. The role of diaspora communities is a rich resource that may not yet be fully engaged by the humanitarian community.
In addition to training and supporting stronger public health systems, humanitarian actors will be required to engage more with governments – something that may challenge the humanitarian principles of neutrality, independence and impartiality. As travel restrictions impact the availability of expatriate staff as well as humanitarian aid, local agencies and staff are one such area where government engagement may be required. While supporting the localisation of humanitarian response, global mobility of the public health workforce to support local health systems will be required to offer support to populations affected by COVID-19. Similarly, supporting equitable access to medical testing and equipment, including vaccinations when they become available, are contributions humanitarian agencies can make.
Already we’re seeing evidence of of individual- and community-level solidarity and acts of kindness, but the travel bans do pose barrier to us realising the most important defence – humanity. As we navigate the new COVID-19 landscape and rise to meet domestic challenges, we must not forget the global citizenship of those experiencing long-term and severe humanitarian need.